Why Dr. John Q. Cook Is the Right Breast Surgeon for You
Our patients benefit from Dr. Cook’s devotion to naturalism and extensive experience with breast surgery. He has performed thousands of operations with breast implants.
Dr. Cook is committed to an individualized analysis of each patient who comes to him for breast augmentation surgery. He considers your breast structure, your goals, and your activity pattern to find a solution that works for you.
We offer our patients a detailed analysis, which includes anatomical breast sizers and simulation software to help you visualize your potential results. We also have an extensive database of before and after photos that our patients have allowed us to share during the consultation process.
Dr. Cook’s experience with complex breast reconstruction surgery provides him with a wide range of technical refinements that he can use to optimize results for his breast augmentation patients.
Education and Credentials

Awards and Recognition

REAL PATIENT RESULTS
See the difference experience makes. View the full before & after photo gallery of Dr. Cook and his team.
Breast Revision
Address Capsular Contracture, Implant Removal, Implant Downsizing, and More to Get the Look You Want for Your Breasts in Chicago and Winnetka
Breast revision surgery at the Chicago-based Whole Beauty® Institute gives breast surgery patients a “second chance” if they are unhappy with the ultimate results of their prior augmentation, lift, reduction, or reconstruction. For more than 20 years, Dr. John Q. Cook has cared for patients who have had a previous procedure and are in need of breast revision, whether because of less-than-ideal cosmetic results, the development of a complication, or even a change in aesthetic taste.
Despite the fact that the motivations behind breast revision can be as varied as implant rippling or rupture, post-reduction “bottoming out,” or reconstruction failure, Dr. Cook has come to recognize common patterns in breast revision surgery. With this in mind, he has assembled a portfolio of techniques to address these patterns, drawing on years of significant medical advances that have improved his success rate in this field.
Breast Revision: Augmentation
Patients seeking augmentation-related breast revision surgery complain of problems that include oversized implants, implant pockets that are too large or in the wrong place, thinning of natural breast structure, overly visible or wrinkled implants, and implant deflation.
There are also breast revision patients whose overlying breast structure has gotten stretched out—usually from natural events such as pregnancy or significant weight loss and weight gain—to where the implant sits at a relatively high position and the natural breast structure has settled to a lower level.
Breast Revision for Downsizing Implants
Breast implant surgery is at its best when it respects and enhances the natural breast structure. There are some patients and doctors who choose implants that overwhelm the breast and are out of proportion with the body structure. The longterm fate of these implants is generally not good, particularly if they are saline implants placed in the subglandular plane. Over time, very large implants produce a predictable set of consequences that prompt patients to consider breast revision: The implant compresses the remaining natural breast structure and causes it to thin out. Because the implants are heavy, the breast skin will stretch, and the breast will settle to a low position. Wrinkles and irregularities will often show through the skin.
There are three main components to a breast revision surgery that corrects oversized breast implants: reducing the implant to a proper size, profile, and shape; restoring proper coverage to the implant; and restoring the breast to a proper position on the body. There is usually a trace of the original breast structure, and Dr. Cook uses this as a guide for breast revision surgery whenever realistic and possible.
Contact Whole Beauty® Institute for more information about breast revision in Chicago or Winnetka. Call 312-751-2112 or send a message online.
Request a consultRead More...
With the breast revision patient’s input, Dr. Cook will select an implant that relates well to the natural breast and body dimensions. If the original implant was salinefilled, he will often recommend conversion to a silicone gel implant. Together, the patients and Dr. Cook will plan the implant’s volume, projection, and shape.
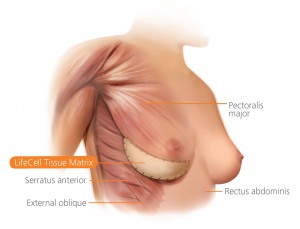
There are several ways to help restore proper coverage to an implant via breast revision, so that there is a layer of natural tissue over the device. Options to consider include moving the implant to the plane under the pectoral muscle, adding thickness with acellular dermal matrix (a biological scaffold), and using fat transfer to restore missing volume in the plane over the remaining breast tissue.
Dr. Cook may recommend some form of breast lift as part of breast revision, both to bring the breast back to a proper position on the body and to reduce the excess stretched-out skin. The good news for patients with oversized implants is that the newer breast revision techniques provide a much better range of choices than used to be the case.
Breast Revision for Reduction or Removal of Normal-Sized Implants
The vast majority of Dr. Cook’s patients maintain a high degree of satisfaction with their implants, even decades after the original surgery. Still, he will occasionally see a breast revision patient who wants to reduce the size of her implants or even remove the implants altogether, even though the original implants respected her natural breast dimensions and body proportion.
Read More...
There are several reasons a breast revision patient might choose to downsize or remove an implant that is relatively good proportion to her body. Some patients gain additional breast structure, either because of hormonal influences or simple weight gain. The additional natural breast structure may simply make the breast larger than the patient desires. These breast revision patients can usually achieve a happy outcome with either a downsizing or a complete removal of the implants, sometimes accompanied by a lift.
A patient’s taste may also change over time. What seemed a perfect volume in her 20s now seems a bit too full, even though the rest of her body’s proportions haven’t changed. Over the years, Dr. Cook has seen a small number of patients who simply don’t like the way implants feel in their bodies. In some cases, it simply makes sense to remove the implants during breast revision surgery.
Breast Revision for Controlling the Space Around Implants to Return Them to their Proper Position
Some patients form almost no scar tissue around their implants. At first glance, this might seem to be desirable, but with no scar to hold the device in place, the normal “wear and tear” of life may cause the implant to shift.
Read More...
Sometimes implant malposition is related to the way the original pocket was created. Dr. Cook has also seen situations where patterns of activity, especially early after augmentation surgery, can move an implant. Structured bras, if worn almost continuously, can help to re-stabilize an implant’s position, but if a patient forms very little scar tissue, even these efforts may not work. For these patients, it is usually necessary to perform breast revision surgery in order to reduce the size of the pocket. This is traditionally done with surgical stitches, but for patients who don’t form much scar tissue, these stitches may pull through.
A variety of surgical scaffolds have increased the probability of success in breast revision surgery to re-position implants. The material can be anchored in place, so that it forms a secure buttress that defines the edge of the pocket and holds the implant in place.
Breast Revision for Correction of Thin Breast Structure
A very thin natural breast structure will reveal an implant’s imperfections, leading many patients to pursue breast revision. One of the worst things about over-sized implants is that they put pressure on the natural breast structure, which causes breast tissue to shrink. This increases the challenge for the surgeon whose mission is to restore the breast to beauty and harmony.
Read More...
Fortunately, plastic surgeons now have a wider range of tools to restore a nice, soft coverage of implants. Autologous fat transfer and acellular dermal matrix have allowed Dr. Cook to increase the thickness of coverage over implants. If the implant has been in the plane above the pec muscle, he will often shift it to the plane under the muscle, which softens what may have been a harsh transition at the upper border of the implant. For some breast revision patients, he uses aspects of the structural breast surgery technique to shift the breast structure to where it is needed.
Breast Revision for Correction of Rippling and Implant Irregularities
There are three main ways that an implant may have visible irregularities or rippling. These irregularities often become more noticeable when a patient leans forward or turns on her side. Some irregularities are caused by the mechanical structure of the implant itself, while others may be caused by the design of the implant pocket. Still others develop due to inadequate thickness of natural tissue over the implant. In general, saline implants are more likely to ripple than silicone gel implants.
Read More...
Some surgeons try to prevent this problem by overfilling saline implants with saltwater, but this produces a hard, ball-like breast. It is also possible to see rippling with silicone gel implants, but this is much less common than with saline implants. The best implants from the standpoint of rippling are the filed with more cohesive gel. These are sometimes called “gummy bear” implants.
Sometimes, the problem driving a breast revision is that the pocket is too large for the implant it holds. This may allow the implant to slide out of position and to ripple, particularly with saline implants. A lack of adequate thickness in the tissue over an implant can also contribute to the problem by allowing irregularities to show through.
Oversized breast implants in effect sabotage their own results, since they tend to cause a thinning out of the natural breast structure. The correction of rippling via breast revision requires an accurate diagnosis of what is causing the problem, so that we can design a strategy for correction of the problem that has the best likelihood of success. Corrective strategies include changing to an implant that is less prone to ripple, controlling the dimensions of the implant pocket, and increasing the thickness over the implant with acellular dermal matrix, fat transfer, and shifting the implant to the space underneath the pectoral muscle.
Breast Revision for Correction of Implant Deflation
If a saline implant deflates, the change is readily apparent, since the breast will visibly lose significant volume. With silicone gel implants, the changes in the breast are subtler. If there is a question of a rupture or shell disruption, the gold standard for diagnosis is an MRI study of the breast. High-resolution ultrasound may also be useful.
Read More...
If an implant deflation occurs, it is not an emergency. With a saline implant breakage, the salt water is simply absorbed by the body. With a gel implant breakage, the natural capsule of collagen that the body forms around the implant keeps everything in place. Also, silicone gel implants from recent years are filled with a cohesive gel that does not tend to drift. Although it is not necessary to rush to surgery, it is also not wise to delay the necessary breast revision procedure for a long period of time, especially with saline implants. If enough time passes, the space around the implant may tighten, making it more difficult for a new implant to create a look that matches the opposite breast.
One question that comes up with breast revision patients in this case is whether it makes sense to simultaneously replace the implant of the opposite breast, which has not deflated. In Dr. Cook’s opinion, if it is just a few years after the first surgery and everything is perfect with the opposite breast, it is reasonable to keep the original implant in place. If a longer period of time has passed—for example, more than 10 years—then it is probably wise to also replace the unruptured implant during breast revision surgery.
Breast Revision for Restoring Proper Relations Between an Implant and a Breast that Has Settled Below It
Life events—such as pregnancy or cycling up and down in weight—may loosen the structure of a breast that sits over an implant. The breast may drift downward while the implant remains in its original position. This produces a breast that has a double contour, with the curve of the implant in the upper area and a second curve formed by the settled breast.
Read More...
If the implant is soft and in a good position, a breast revision involving a lift will restore a proper balance between the breast and the implant by bringing the breast back to its proper position over the implant. Dr. Cook evaluates each breast revision patient in detail to determine which lift technique is best suited to her breast structure and her goals. Options include the periareolar lift, the classical (anchor) lift, and the structural lift.
Breast Revision: Lifts
Breast revision patients seeking help after a lift come to Dr. Cook for several reasons. The most common is a recurrence of the ptosis (or drooping) that originally prompted them to seek surgery. This is accompanied by a hollowing out of the upper portions of the breast structure. There may also be a stretching out of the skin of the lower portion of the breast.
Some patients considering breast revision are most concerned with a lack of good tone to the breast. Others may lack sufficient volume and desire an overall breast enlargement. Dr. Cook has also seen breast revision patients who desire improvement in the appearance of the scars from the original surgery or who would like to alter the position and size of the areola.
For patients who have undergone a breast lift, only to see the breasts settle back toward their original position, the change may be related to the fact that the original procedure relied only on the skin to lift the breast. Whenever possible, Dr. Cook relies on structural techniques for the breast revision surgery, since this strategy provides additional anchoring of the breasts at deeper levels. He may also be able to shift some of the breast structure to the upper portion of the breast so that the hollowness in this area is corrected.
Some patients who desire breast revision surgery after a lift are in need of more volume. For these patients, Dr. Cook will usually make use of implants and also tighten the breast structure. The consultation will include a thorough discussion of implant type, shape, and position in order to develop the best treatment plan.
Some breast revision patients have previously undergone a breast augmentation with lift and now have breasts that are stretched out in their lower portions. This may be particularly true if implants were placed in the plane under the breast (as opposed to under the muscle). If the implants were not properly supported in the original operation, it may be necessary for Dr. Cook to move them to the plane under the muscle and support them with acellular dermal matrix or other surgical scaffolding. The overlying breast structure can then be re-contoured during breast revision surgery so that it properly covers the implant.
Breast Revision: Reduction
Bottoming out after surgery is probably the most frequent reason breast revision patients come to see Dr. Cook after reduction surgery. Over time, the weight of the tissue that remains after a reduction procedure may stretch the skin of the lower part of the breast. This allows the breast tissue to droop downward, usually with a hollowing out of the upper part of the breast. The nipple and areola take on an upward tilt and sometimes rise to a level that can be embarrassing when seen in certain outfits and swimsuits.
Dr. Cook analyzes each patient on an individual basis in order to come up with the best treatment plan for bottoming out. For some breast revision patients, a nice improvement can be obtained if he removes skin according to the original surgical pattern. The fold under the breast may need to be stabilized, and sometimes the full lower part of the breast needs to be stabilized with acellular dermal matrix or mesh.
The breast is a structure that responds to the hormonal environment of the body as well as weight gain and weight loss. Some breasts may be an ideal size after breast reduction surgery—but then become larger over the years. For some breast revision patients, growing breasts may have reached a size where they require further reduction.
There are many different ways to sculpt breast tissue in breast revision surgery for reduction. The precise method of sculpting may not be predictable from the scars on the surface of the breasts. The way the tissue was sculpted by the original surgeon may have significant implications for blood supply to the nipple if further sculpting is carried out in a breast revision procedure. For this reason, it is very important for patients to provide Dr. Cook with a copy of the original operative report if they desire further reduction during their breast revision procedure.
On the other end of the scale, some breast revision patients have too little breast tissue after reduction surgery, either as a result of the original operation or as a result of changes in the breast over time.
It is very common for patients to lose significant weight after breast reduction, since the operation improves body mechanics and makes exercise more pleasurable. Often, a virtuous cycle is created where there is a self-reinforcing desire for increasing levels of exercise. This, of course, is wonderful for the patient—but may have negative consequences for the shape of the breast. This is particularly true for fatty breasts, which tend to respond more to overall weight loss and weight gain than glandular breasts.
Breast revision surgeries for breasts that are deficient in volume after a reduction procedure usually involve the placement of implants. The size, type, and position of the implants are determined as part of a detailed discussion of the patient’s goals. The previous pattern of sculpting may also affect Dr. Cook’s choice of implant placement. For some patients, fat transfer may be an option. As part of an overall artistic assessment of the breast, he may also adjust the balance of the breast skin and the position of the areola.
Most patients heal beautifully after reduction surgery, but as with any surgical procedure, the scars may be less than ideal. The most frequent area for breast revision is the scar that runs around the areola, as it can sometimes spread or create a zone of whiteness that is embarrassing to the patient. Other reduction surgery scars can also spread. In some patients, the lower pole of the breast slips below the original scar from the surgery, in which case it may be desirable to reset and anchor the scar in the proper position with breast revision. If the patient simply needs a revision of the scars without any other modification of the breast structure, this can often be done under local anesthesia in the office.
Breast Revision: Reconstruction
Breast revision patients who come to Dr. Cook after breast reconstruction often have a combination of issues that need to be resolved. This is particularly true for patients who have had a one-sided reconstruction.
As a general rule, if a patient has undergone a double mastectomy and reconstruction and has not been treated with radiation, the two breasts will behave similarly as time passes. On the other hand, if the patient has undergone a one-sided mastectomy and reconstruction, the two breasts will behave differently as time passes, even if there was nearly perfect balance when the reconstruction was completed.
Dr. Cook has helped breast revision patients with a wide variety of long-term postreconstruction issues. These include capsular contracture (a tightening of scar tissue around the implant), an abnormal shape to the reconstructed breast, an imbalance of size or position between the reconstructed and the natural breast, a harsh transition at the edge of the breast implant, implant rippling or irregularity, excess fullness in the upper portion of the reconstructed breast, or failure of a previous reconstruction.
Each of these issues requires a breast revision approach that is based upon considerable skill and experience in techniques of reconstructive breast surgery. The good news is that a variety of advances in implant design and surgical technique increases the odds of achieving a good natural shape and balance between the two breasts. These advances include acellular dermal matrix, autologous fat transfer, and form stable implants.
Read More...
The Consultation for Breast Revision After Reconstruction
The breast revision consultation is a sharing of information. Dr. Cook learns the patient’s general state of health, her priorities for the reconstruction, and her pattern of living and activity, since these elements may influence the choice of breast revision techniques.
Dr. Cook then makes a careful list of the issues he sees in the reconstructed breast and discusses potential improvements. Since he has a referral practice, he sees quite a few patients for breast revision surgery in a given year. For these patients, he emphasizes a practical, goal-oriented approach.
Above all, the patient must accept that although we can usually obtain a significant improvement, it is never possible to reach perfection. “Better, but not perfect” is a point that Dr. Cook repeatedly emphasizes with his breast revision patients.
Breast Revision for Correcting a Reconstructed Breast that Is Smaller and Higher than the Natural Breast
Asymmetry is a common pattern that Dr. Cook sees in patients who are referred to him for breast revision surgery after reconstruction. If the limiting factor is the tightness of the capsule around the reconstructive implant, but the skin of the breast is not tight, he can usually open up space for a larger implant by removing the capsule of scar tissue and placing acellular dermal matrix or other scaffolding between the bottom edge of the pectoral muscle and the fold under the breast.
He will typically place a cohesive gel implant and carry out fat transfer for this breast revision procedure and will modify the opposite natural breast so that it is lifted to a better position. If necessary, he will also reduce the volume of the breast to get the best possible match with the reconstructed side. If the skin of the reconstructed breast is too tight, there are two options.
Breast Revision for Correcting Reconstructed Breast Irregularities
There are several possible causes for visible irregularities, such as rippling in breasts that have been reconstructed with implants. In general, saline implants are more likely to show rippling and irregularity than silicone gel implants.
Sometimes, there is a mismatch between the implant and the space where the implant sits. If the pocket is too small relative to the base dimension of the implant, the proportions will cause the implant to fold and wrinkle. Too large a pocket can also allow the implant to shift out of alignment and develop wrinkles.
Patients who have very little structure over the implant also are more likely to show imperfection. Dr. Cook selects a breast revision strategy based upon his assessment of the most likely cause of the rippling, but he is prepared for extra measures in case he finds other causes once he explores the pocket where the implant lies.
In general, Dr. Cook has found that cohesive gel implants are less likely to wrinkle than other types of implants, and silicone gel implants are less likely to ripple than saline implants.
Adjustment of the implant pocket, which may require acellular dermal matrix or other scaffolding, is often an important step in breast revision. It is also possible to provide extra structure for breast revision patients who have extremely thin coverage over their implants. This can be accomplished either with a fat transfer procedure or by placing a sheet of acellular dermal matrix over the implant.
Breast Revision for Correcting Excessive Fullness in the Upper Portion of a Reconstructed Breast
Reconstructed breasts are more likely to be too full in their upper portions than natural breasts that have been augmented. There is less tissue to camouflage the upper border of the implant with mastectomy. The lower portion of the reconstructed breast can also be tight, which pushes the implant toward the upper portion of the breast.
Fortunately, several recent innovations in reconstruction surgery give us a better chance to use breast revision to restore a normal shape to reconstructed breasts so that there is a natural curve in the lower portion of the breast and an upper part of the breast that is not too full.
Form-stable implants are made of highly cohesive silicone gel so that they maintain a natural shape. For some patients, conversion to a form-stable implant may be helpful.
A breast revision procedure that includes fat transfer can add volume to the lower portion of the reconstructed breast and also soften the transition at the upper edge of the implant.
Acellular dermal matrix and other surgical scaffolding can open up the space at the lower portion of the reconstructed breast so that a form stable implant can achieve optimum fullness.
Breast Revision for Correcting Failed Breast Reconstruction
When a patient is referred to a plastic surgeon with a failed breast reconstruction, the first priority is to determine the cause of the failure. Once the surgeon understands this cause, he or she can devise a breast revision plan that provides the best chance of success.
One cause of failure is infection. If there is a skin-level infection of a reconstructed breast (cellulitis), the problem can usually be brought under control with antibiotics—no need to remove the implant. If there is an infection at the level of the implant, however, it is usually necessary to remove the device to bring the infection under control. Once the infection is cleared, it is usually possible to obtain a good quality reconstruction via breast revision surgery. There are many possible options, including the use of flaps, the placement of tissue expanders, and fat transfer.
Breakdown of the skin over an implant can also lead to the failure of reconstruction results. The breakdown usually occurs along an incision line, although it is possible for it to develop anywhere the skin is very thin. The likelihood of a breakdown increases significantly if the area has been radiated. If the implant has not yet been exposed and there is no sign of infection, it is usually possible to salvage the situation during breast revision. For most patients, this is best done by the original reconstructive surgeon. The specific strategy will be determined by the patient’s individual circumstances.
Breast revision options include flaps, reinforcing the area with acellular dermal matrix, fat transfer, and the placement of an expander to take pressure off of an area of weakness. If the previous surgeon had to remove an implant, all is not lost. Sometimes it is desirable to bring in additional tissue with a flap. Often, the disadvantages of a flap can be avoided with a series of fat transfers to restore quality and thickness to the breast skin. For some patients, tissue can be modified with a preliminary external skin-stretching device.
Once the surgeon has prepared the breast skin in this manner, he will place an expander and re-stretch the breast structures. When the expansion portion of the breast revision is complete, he will place an implant. Acellular dermal matrix frequently helps to provide additional internal protection of the implant.
Dr. Cook performs surgery for revision of breast reconstruction on an outpatient basis. If he sees a patient who will require methods such as microvascular free tissue transfer or flap surgery, he will refer to colleagues in the Division of Plastic Surgery at Rush University Medical Center.
Breast revision surgery taxes the ingenuity of the surgeon and may require several operations, but the newer techniques have significantly increased the odds of success. Breast revision surgery can provide significant improvement in a patient’s quality of life.
Breast Revision and Skin-Stretching Techniques
For years, tissue expanders have been key devices for breast reconstruction. The expander is placed under the skin and pec muscle, where it gradually expands with weekly injections of salt water through a valve. This prepares a space for the reconstructive implants.
As fat assumes a greater role in reconstruction, the preparation of a space to accommodate the fat becomes very important. There are external devices that allow the plastic surgeon to stretch the skin of the chest area, so that it is optimized to receive transferred fat. This may be helpful in complex reconstruction and breast revision surgeries.
What Advanced Breast Revision Tools Does Dr. Cook Use?
Like all surgeries, breast revision requires an accurate diagnosis of the problems a patient is experiencing and a series of steps that will provide an improvement. There are several developments in the field of breast revision surgery that have opened up possibilities for helping patients who require breast revision. These developments include acellular dermal matrix, form stable implants, autologous fat transfer, and structural techniques of breast surgery.
Read More...
Acellular Dermal Matrix for Breast Revision
Acellular dermal matrix and other surgical scaffoldings have several useful roles in breast revision surgery. For breasts that have become stretched out in their lower portion, these materials can help to support the breast structure in a new position. For implants that have moved out of position, they can help to stabilize the pocket for the implant.
Acellular dermal matrix can also be used in breast revision to help camouflage irregularities that sometimes occur with implants in thin patients, especially in breast reconstruction.
Acellular dermal matrix can also be very helpful for breast revision patients who have developed capsular contracture around their implants. The body sometimes develops a tight pocket of scar tissue around an implant, which can distort the breast shape and cause the breast to be unusually firm.
Like many surgeons who do breast revision surgery, Dr. Cook has been impressed by the ability of acellular dermal matrix to prevent the return of capsular contracture. The strategy is to cover a portion of the implant with the acellular dermal matrix, which seems to prevent the body from making scar tissue at this location. This “loosens the grip” of any capsule that may form.
Highly Cohesive Gel Implants for Breast Revision
Implants that contain highly cohesive silicone gel tend to maintain their shape and projection and are less prone to rippling than implants filled with thinner gel. They are sometimes referred to as “gummy bear” implants. Patients today are fortunate to have a wide variety of implant shapes, cohesivity and projection. Consideration of these factors is an important part of planning a revision procedure.
Autologous Fat Transfer for Breast Revision
Dr. Cook’s familiarity with techniques of fat transfer is extensive, since he has used the procedure to restore volume in his facial rejuvenation
patients for more than 15 years.
In recent years, he has employed fat transfer to the benefit of his breast reconstruction and breast revision patients. Fat is a remarkable tool, because it can be used restore or add volume to very specific areas.
It can help to camouflage implants, particularly in thin people. Fat can also be used to improve the quality of skin that has been irradiated.
Structural Breast Surgery for Breast Revision
The development of structural breast revision techniques has been a major project of Dr. Cook’s for many years. The rearrangement of breast structure to restore natural volume to the upper portion of the breast and the deep structural anchoring of the breast can be very useful in a variety of circumstances when he revises the results of previous breast surgery.
If you would like to have a consultation regarding breast revision in the Chicago, Hinsdale, and Winnetka areas, or if you have questions for our team, please call 312-751-2112 or contact us online.
Request a consult
Capsular Contracture After Augmentation with Implants: What Is It and How Is It Treated?
During the healing process after breast augmentation surgery, a normal and beneficial part of the recovery includes the development of scar tissue that forms around the implant. The benefits to this are the scar tissue helps to hold the implant in place, and it helps...

Will My Breast Implants Feel Natural?
The latest options for breast implants and surgical techniques make modern breast augmentation more advanced and better for patients than the surgery ever has been before. There are many advantages to this procedure, including the fact that it can enhance your...

What Can You Do to Prepare for Breast Augmentation?
Breasts have been considered a symbol of beauty, motherhood, and vitality for centuries in most cultures. With that in mind, some women find that enhancing the size of their breasts through breast enhancement from our Chicago-based Whole Beauty® Institute brings them...

Preparation and Recovery for Breast Reduction Surgery
The decision to undergo breast reduction surgery is important. In order to help you optimize your surgical experience, I have put together some suggestions for preparation and recovery for breast reduction surgery.

How Do You Know if You Need a Breast Lift?
Breast sagging, otherwise known as breast ptosis, is a common condition that occurs as your breasts begin to droop over time. Just like any other area on your body, the breasts will go through changes as you age. There are several potential causes, including a loss of...

Which Breast Implants Feel More Natural?
Many patients wonder if it is possible to have natural-feeling breasts after breast augmentation. They may think that placing a breast implant under the breast automatically makes the breast feel fake or hard. Fortunately, improvements to breast augmentation...

Answers to the Top Breast Augmentation FAQs: Part 2
The Whole Beauty Institute believes in empowering patients through education, transparency and clear communication. Our website includes other valuable information about breast augmentation, including our pages on ten questions to ask a surgeon during your breast...

Choosing a Breast Augmentation Surgeon You Can Trust
While many factors contribute to a successful breast augmentation surgery, the right surgeon is undoubtedly one of the most important yet least discussed. Since breast augmentations are such a common cosmetic procedure, it is easy to assume that any plastic surgeon...
Practice Blog
Learn more about Dr. John Q. Cook and the non-surgical treatments and plastic surgery procedures available at The Whole Beauty® Institute. Get tips and advice, discover new ways to improve your health and beauty, and more.
Dr. Cook's HealthGems Blog
Dr. John Q. Cook shares his personal thoughts on well-being, quality of life, and more—all drawn from his decades of experience in the industry, studying and working with advanced technology and techniques.
Whole Beauty Skincare
SkinShopMD was created by board-certified plastic surgeon John Q. Cook, M.D. as a trusted source for skin care products. From his years of experience, he developed a portfolio of high quality medical grade products to protect and rejuvenate your skin.

Educational Information
Learn important information about surgical and non-surgical procedures to help you make informed decisions about your desired treatment based on your goals. Topics cover facial surgery, injectables, lasers, breast surgery, body contouring, and other treatments.
Testimonial and Practice Videos
Schedule a Consultation
Schedule a consultation with board-certified plastic surgeon, John Q. Cook, M.D., to learn more about plastic surgery solutions that may be right for you based on your aesthetic goals.
"*" indicates required fields
Our Office Locations
Our locations in the Gold Coast of Chicago and Winnetka in the North Shore reflect our commitment to convenient and discrete concierge-level service.
Chicago Office
737 North Michigan Ave., Suite 760 Chicago IL 60611 (312) 751-2112 Entrance at 151 E. Chicago Avenue
Winnetka Office
118 Green Bay Road Winnetka IL 60093 (847) 446-7562
Located directly across from Indian Hill Metra Station